- Clinical Image
- |
- Open Access
Benign stromal tumor: Breast images
- Maha Abdel Hadi;
- Department of Surgery, Imam Abdulrahman Bin Faisal University, Saudi Arabia
- Weddad Bagatada;
- Department of Radiology, Imam Abdulrahman Bin Faisal University, Saudi Arabia
- Hassan Al Ahmadi
- Department of Pathology, Imam Abdulrahman Bin Faisal University, Saudi Arabia

| Received | : | Oct 25, 2018 |
| Accepted | : | Feb 11, 2019 |
| Published Online | : | Feb 15, 2019 |
| Journal | : | Annals of Breast Cancer |
| Publisher | : | MedDocs Publishers LLC |
| Online edition | : | http://meddocsonline.org |
Cite this article: Hadi AM, Bagatada W, Ahmadi AH. Benign stromal tumor: Breast images. Ann Breast Cancer. 2019; 2(1): 1008.
Clinical Image Description
A 70 years old female of suburban descent presented to the breast specialty clinic with 10 years history of a left enlarging painless breast mass not associated with local or systemic symptoms. There were no associated comorbidities or family history of breast cancer. Systemic examination was unremarkable. Local breast examination revealed obvious breast asymmetry with a large 10 × 11-centimeter smooth, non-tender, mobile mass occupying the retro-areolar and central regions of the left breast. The overlying skin was stretched over the lesion with tortuous dilated superficial veins. No palpable axillary lymphadenopathy (Figure 1).
Figure 1: Showed obvious asymmetry between the two breasts with no evidence of skin or nipple changes.
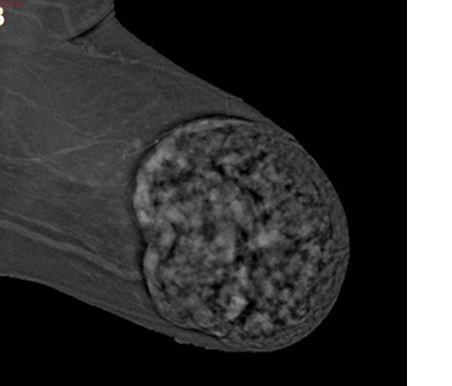
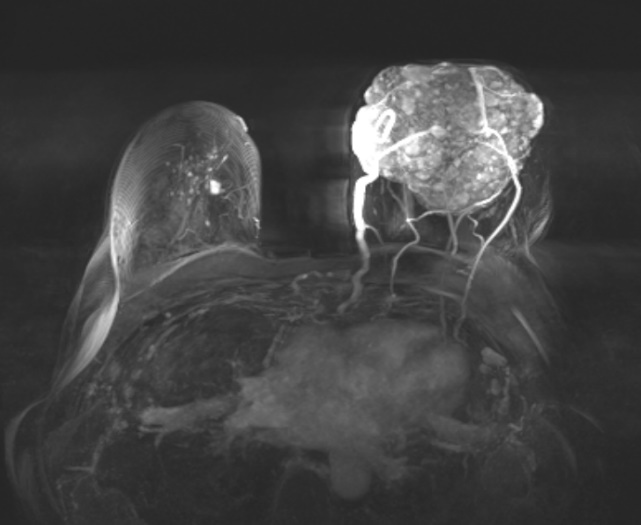
Breast images suggested the benign nature of the lesion based on the breast ultrasound which showed an out of range solid breast lesion with intact capsule, Contrast Mammography (Figure 2) demonstrating the well circumscribed nature of the mass and further confirmation by MRI that depicted the abundant peripheral blood supply (Figure 3).
Figure 2: Contrast enhancing left mammogram demonstrating the well circumscribed breast lesion with thicked capsule.
Figure 3: MRI showing a large well-defined lobulated progressively enhancing mass with non-enhancing septa is occupying anterior and mid breast with dilated peripheral feeding blood vessels.
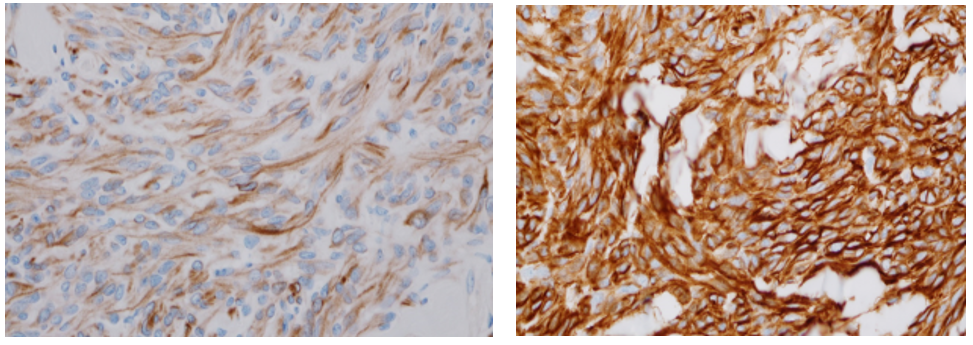
Core biopsy was reported as spindle cells infiltrating the fibrous tissue in both linear and curvy-linear fashion. Nor mitosis or necrosis were identified.
Patient underwent Complete surgical excision with ease leaving grossly normal compressed breast tissue in the cavity. The striking intraoperative findings was a well capsulated soft tissue mass with large tortuous blood supply running along the peripheral surface of the lesion (Figure 4).
Immuno-histological staining was reported as ER +ve, PR+ve, Her2 -ve with Ki67 5%. The presence of desmin and CD34 suggested the final diagnosis of the rare Mammary Myofibroblastoma (Figure 5ab).
Recurrence is unlikely following wide local excision with clear resection margins.
Acknowledgement
Special appreciation to Dr. WeddadBagatada and Dr. Hassan AlAhmadi for contributing in radiology and pathology materials.
MedDocs Publishers
We always work towards offering the best to you. For any queries, please feel free to get in touch with us. Also you may post your valuable feedback after reading our journals, ebooks and after visiting our conferences.