Annals of Bariatrics & Metabolic Surgery
HOME /JOURNALS/Annals of Bariatrics & Metabolic Surgery- Research Article
- |
- Open Access
Consensus survey on mini-gastric bypass and one-anastomosis gastric bypass
- Mervyn Deitel;
- MGB-OAGB Club, Canada
- Kuldeepak S Kular;
- MGB-OAGB Club, Kular College & Hospital, India

| Received | : | Apr 22, 2018 |
| Accepted | : | May 11, 2018 |
| Published Online | : | May 16, 2018 |
| Journal | : | Annals of Bariatrics & Metabolic Surgery |
| Publisher | : | MedDocs Publishers LLC |
| Online edition | : | http://meddocsonline.org |
Cite this article: Deitel M, Kular KS. Consensus survey on mini-gastric bypass and one-anastomosis gastric bypass. Ann Bariatr Metab Surg. 2018; 1: 1001.
Abstract
Introduction: An online questionnaire was filled out by pre-registered experienced attendees prior to the Annual Mini-Gastric Bypass (MGB) – One-Anastomosis Gastric Bypass (OAGB) Conference held at Naples, Italy, July 2017.
Methods: Data on the MGB and OAGB were compiled and analyzed, and the sequelae were tabulated. World literature was also reviewed.
The reports of the 139 respondents indicated that the MGB and OAGB are favorable operations with respect to safety, resolution of co-morbidities (especially diabetes), short learning curve, and durable weight loss. We derived some guidelines from these results.Conclusion: MGB and OAGB are favorable bariatric operations, but follow-up is required.
Keywords: Mini-Gastric bypass; One-Anastomosis gastric bypass; Morbid obesity; Bariatric surgery; Consensus survey; Post-Operative complications; Results on obesity-related comorbidities; MGB-OAGB guidelines
Introduction
Mini-gastric Bypass (MGB or Malabsorptive Gastric Bypass) was devised by Rutledge in the USA in 1997. As a trauma surgeon, he was faced with an abdominal gun-shot wound, where duodenal exclusion with a Billroth II anastomosis was an appropriate reconstruction. This was the inspiration for the MGB, constructing a long lesser curvature channel which inhibits Gastro-Esophageal Reflux (GER) [1] (Figure 1).
Figure 1: MGB created by horizontal division 2-3 cm distal to crow’s foot, and then vertical stapler-division upwards (~18 cm), dividing to the left of the angle of His. A wide antecolic gastrojejunostomy (GJ) is performed ~200 cm (varied with BMI) distal to Treitz’ ligament, providing malabsorption.
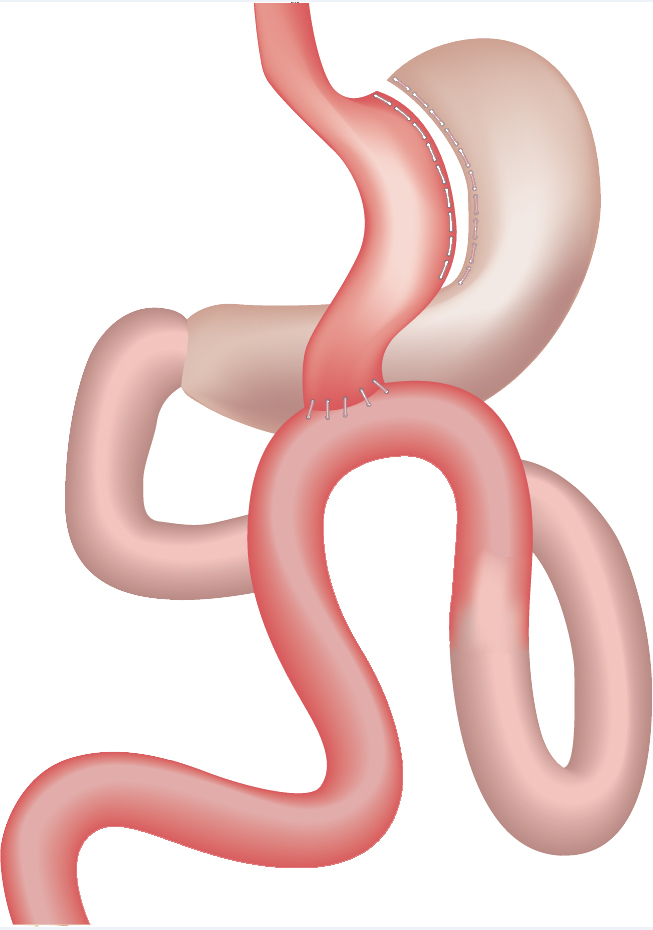
Because of suspected GER, in 2002 a variant of the MGB, named One-Anastomosis Gastric Bypass (OAGB) or BAGUA (Bypass Gastrico de Una Anastomosis) originated in Spain by Carbajo and Garcia-Caballero [2] (Figure 2). Previously, they had performed the Roux-en-Y gastric bypass operation (RYGB) for >10 years.
Figure 2: OAGB with a 15-18 cm gastric pouch and a 2.5 cm latero-lateral anastomosis between pouch and afferent jejunal loop which is suspended above the anastomosis by an initial continuous suture which secures the loop to the gastric pouch’s stapleline, with final fixation of the loop’s apex to the bypassed stomach. Biliopancreatic limb averages 250-350 cm (diagram by Dr. Arturo Valdes Alvarez of Saltillo, Mexico).
The MGB and OAGB have been increasing throughout the world [3-9], and in 2015 became the third most common bariatric operation internationally [10].
Methods
Annual conferences on MGB and OAGB had been held in Paris, India, Montreal, Vienna and London, where the MGB-OAGB Club was formed [11].
A carefully designed questionnaire was posted on the Club website and also emailed to surgeons who had performed MGB or OAGB, and who had pre-registered for the MGB-OAGB Club Conference in Naples in 2017. A total of 139 surgeons from 31 countries who had performed 100 or more MGBs or OAGBs for one or more years were elgible and completed the survey. These surgeons kept accurate records, because the MGB-OAGB had met with some prejudice in early years. The survey compared the results of 37, O94 MGBs and the 9,203 OAGBs performed by the participants, which is the biggest report to date.
Of the 139 respondents, 128 had been performing the MGB or OAGB as their principal bariatric operation: 17 (12%) of respondents had performed >1,000 MGB-OAGB operations, 15 (11%) had performed 500–1000, and 107 (77%) had done 100–499 MGB-OAGBs. Data is reported as frequency, percentage, mean and standard deviation of valid responses. A p-value <0.05 using unpaired t-test was considered significant.
Results
In the reported 37,094 MGBs and 9,203 OAGBs, the mean pre-operative BMI was 45.2 kg/m2 and 44.3 kg/m2 respectively, and the mean age was 43.5 and 44.2. Mean 30-day mortality rate was 0.03% and 0.01% in MGB and OAGB respectively. The leak rate in MGB and OAGB was 0.4 and 0.34% respectively. The survey data are shown in Table 1.
Post-operative changes are shown in Table 2, and found similar results between the two operations. At 5 years, 85.1% of patients who had undergone MGB had >50% Excess Weight Loss (EWL) using Metropolitan Life statistics [12]. At 5 years, 87.4% of patients who had undergone OAGB had >50% EWL.
Effect of gastric pouch length, diameter of Gastro-jejunostomy and bypass length on various parameters in MGB and OAGB
Of the 139 respondents, 91% reported that they begin the gastric pouch below the crow’s foot, 6% at the crow’s foot and 3% above the crow’s foot. Of the 920 (0.02%) MGB revisions reported for intractable bile GE Reflux (GER), most were patients with a short pouch (starting at or above crow’s foot). With the OAGB, surgeons reported no revisions for GER.
The gastric pouch was constructed loosely around a 32-42Fr bougie by 66%, but 19% constructed a tight pouch against the bougie (as in laparoscopic sleeve gastrectomy – LSG), and 12% a wide pouch (1-2 cm away from the bougie).
Regarding biliopancreatic limb-length (ie. bypass length), 53% chose 150-200 cm, 31% chose 201-250 cm, 10% chose 251-275 cm (mainly the OAGB surgeons), and 6% chose a tailored length depending on the BMI. At 1 year, in patients with >200 cm afferent limb, mean %EWL was 81.4%, and in patients with <200 cm afferent limb, %EWL was 77.5%. At 5 years, with either afferent limb lengths, EWL was similar: 75.2% in patients with the longer limb (>200 cm) and 74.0% in patients with the shorter limb.
For the MGB, the intended diameter of the Gastro-Jejunostomy (GJ) was 6 cm for 18%, 4-5 cm for 47%, and 3-4 cm for 35% of the respondents (Table 3). The OAGB surgeons reported an anastomotic diameter of 2.5-3cm.
In patients with pre-existing Hiatus Hernia (HH) and GERD, 72% of MGBs were performed without repairing the HH, because of data showing that MGB improves GE reflux [13,14]. However, with a significant HH and reflux, 18% recommended HH repair or RYGB at the time of MGB. Most OAGB surgeons repaired a HH if present.
Discussion
The MGB has two components: 1) a lesser-curvature long gastric pouch, serving as a slightly restrictive conduit, allowing adequate oral intake; 2) a180-200 cm jejunal bypass with a wide ante colic GJ anastomosis, which results in carbohydrate and fat malabsorption [13]. A32-42 (mean 38) Fr bougie was passed by the anesthesiologist, and the stomach was stapler-divided cephalad, going ~1cm lateral to the angle of His; the cardia and left crus are not dissected, unlike in the LSG. Thus, in the MGB, a low-pressure gastric conduit is constructed [14], unlike the high-pressure conduit of the LSG [15].
In super-obese patients, 250 cm of proximal jejunum may be bypassed. In lower BMI with co-morbidities such as diabetes, 150 cm may be bypassed [13,16,17]. At the selected site, the tip or adjacent posterior wall of the gastric pouch is anastomosed ante colic to the jejunum, constructing a wide anastomosis under easy view. The GJ anastomosis should be at least 300 cm proximal to the ileocecal valve, to avoid protein malnutrition.
As stated, a HH was generally not repaired at the time of MGB. If needed (which was infrequent), HH repair was performed 12-18 months postoperatively [18]. However, for large HHs with adherence to gastric fundus, dissection and repair were performed at the time of MGB.
Patients avoid carbohydrate which could produce rapid dumping; thus, the food intake has mainly malabsorption of fat. The pouch in the MGB develops minimal dilatation, because there is no gastric outlet narrowing [14].
If ever necessary, the MGB can be modified by moving the GJ anastomosis distally or proximally [19]. The MGB can be easily reversed in rare cases of intractable hypoalbuminemia or excess weight loss by stapler-division along the GJ anastomosis (carefully inspecting the jejunal side), linear anastomosis of the gastric pouch to the matched bypassed stomach, and closing the defect at the bottom of the gastric pouch with running suture [18].
The OAGB variant of the MGB has a similar malabsorptive component [2,9]. In the OAGB, a side-to-side anastomosis of the afferent limb to the gastric pouch (rising on the remnant stomach), facilitates emptying of biliopancreatic juices toward the efferent limb, preventing GER. In >2,000 patients, Carbajo has not needed to revise any OAGB for reflux, as in our study
The MGB, with the long gastric conduit, was found in our study to have a GER problem in 0.07%; if GER occurs, the patient should be questioned about smoking and taking non-steroidalantiinflammatory drugs (which are prohibited), eating late at night, and lots of fried foods. It may be treated conservatively, or by Braun jejuno-jejunostomy or RYGB. The OAGB took slightly longer to perform (and is slightly more difficult to reverse) than the MGB. The OAGB represented 19.9% of the single anastomosis gastric bypasses in our study.
The rare leaks in our survey were usually at the GJ, and were far less than the troublesome proximal leaks following LSG [20]. Patients were usually ambulatory a few hours after surgery.
In USA, Hargroder had no operative deaths (i.e. within 30 days) in 1,450 patients over 13 years of MGB, and Peraglie had no operative deaths out of 1,800 MGBs over 13 years [21]. Furthermore, Peraglie found no deaths in his super-obese patients [22] and those age >60 [23].
GER resolved in the majority (>70%) after MGB (Table 2), explained by the decrease in gastro-esophageal pressure gradient after MGB [14].
Table 3: Relationship between stated diameters used for Gastro-Jejunostomy (GJ) and %EWL at 1 and 5 years after the MGB.
It was noted after MGB-OAGB (as after RYGB) that alcohol is absorbed intestinally fairly rapidly. If persisting dyspepsia occurs post-operatively, H. pylori (HP) or pouch kinking should be ruled out. HP stool antigen or breath test was often checked pre-operatively and eradicated if positive. If there is indigestion or marginal ulcer, a proton pump inhibitor was prescribed (sometimes routinely).
After MGB-OAGB, supplements consisted of multi-vitamins, calcium (dairy or calcium citrate), yoghurt, vitamin D3 1,000 IU 2-3 times daily, sublingual crystalline B12, and an intestinally-absorbed iron supplement (Proferrin® –heme intestinal peptides). In 5% of menstruating women, iron deficiency was reported and required increased oral iron or rarely IM or IV iron [24].
Fruits and salads are well tolerated. Foods containing protein were important, eg. meats, seafood, nuts and dairy. No intractable hypoglycemia was reported. Fried and fatty foods caused cramps and diarrhea (steatorrhea) and are avoided. Vegetarians must take protein –legumes (lentils, beans, chick peas, peanuts, quinoa), yoghurt, milk, soy (tofu) or whey protein. In vegetarians and the elderly, it was advisable to bypass <200 cm of jejunum to avoid hypoalbuminemia [17].
After RYGB, lap-band or LSG, carcinoma in the stomach and lower esophagus has been reported in 46 patients [25-27]. After LSG, Barrett’s esophagus is frequent [28]. After MGB or OAGB, no carcinoma in the gastric pouch or esophagus has been reported. However, in the Far East (Taiwan) where the incidence of gastric carcinoma remains high, one carcinoma 9 years after MGB has been reported in the bypassed stomach (but not in the pouch) [29].
After LSG [20,30] and RYGB [31], significant weight regain has been found in the long-term. Comparative studies have documented more durable weight loss after the MGB [32-34]. Better quality of life has been found after MGB [35]. Diabetes, hypertension and lipid abnormalities have shown superior remission after MGB and OAGB [36,37]. Diabetes resolved in 79- 94% after MGB [17,38-40]. Likewise, after OAGB, resolution of type 2 diabetes and other co-morbidities were found [41,42], including in the massively obese adolescent [43]. In diabetic patients with BMI <35, Kular found that HbA1c at 7 years after MGB was 5.7 ±1.8% [44].
Conclusion
The survey has indicated that MGB and OAGB are rapid, and technically simple and relatively safe bariatric operations. The jejunal bypass length is modifiable with the degree of BMI. The MGB-OAGB show co-morbidity resolution and durable weight loss. The single non-obstructing ante-colic GJ constructed in easy view provides a technically easy option for revision or reversal. The MGB and OAGB patient should be monitored for possible development of hypoalbuminemia and iron deficiency.
References
- Rutledge R, Walsh W. Continued excellent results with the minigastric bypass: six-year study in 2,410 patients. Obes Surg. 2005; 15: 1304-1308.
- Garcia-Caballero M, Carbajo MA. One anastomosis gastric bypass: a simple, safe and efficient procedure for treating morbid obesity. Nutr Hosp. 2004; 19: 372-375.
- Lee WJ, Yu PJ, Wang W, Chen TC, Wei PL, Huang MT. Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity: a prospective randomized controlled clinical trial. Ann Surg. 2005; 42: 20-28.
- Rutledge R. Revision of failed gastric banding to mini-gastric bypass. Obes Surg. 2006; 16: 521-523.
- Chevallier J-M, Chakhtoura G, Zinzindohoue F.Laparoscopic mini-gastric bypass. In: Deitel M, Gagner M, Dixon JB, Himpens J, editors. Handbook of Obesity Surgery. Toronto: FD-Communications. 2010: 78-84.
- Noun R, Skaff J, Riachi E, Daher R, Antoun NA, Nasr M. One thousand consecutive mini-gastric bypass: short and long-term outcome. Obes Surg. 2012; 22: 697-703.
- Musella M, Sousa A, Greco F, De Luca M, Manno E, Di Stefano C, et al. The laparoscopic mini-gastric bypass: the Italian experience: outcomes from 974 consecutive cases in a multi-center review. Surg Endosc. 2014; 28: 156-163.
- Kular KS, Manchanda N, Rutledge R. A 6-year experience with 1,054 mini-gastric bypasses – first study from Indian subcontinent. Obes Surg. 2014; 24: 1430-1435.
- Carbajo MA, Luque-de-Leon E, Jiminez JM, Ortiz-de-Solorzano J, Perez-Miranda M, Castro-Alija MJ. Laparoscopic one-anastomosis gastric bypass: technique, results, and long-term follow-up in 1200 patients. Obes Surg. 2017; 27: 1153-1167.
- Deitel M. Letter to the editor: bariatric surgery worldwide 2013 revealsa rise in mini gastric bypass. Obes Surg. 2015; 25: 2165.
- Deitel M, Kular KS, Musella M, Carbajo M, Luque-de-Lyon E. A new organization – The MGB-OAGB Club. Bariatric News. 2016; 26: 10.
- Deitel M, Gawdat K, Melissas J. Reporting weight loss. Obes Surg. 2007; 17: 565-568.
- Rutledge R, Kular KS, Chiappetta S, Manchanda N. Understanding the technique of MGB: clearing the confusion. Chapter 1. Deitel M, ed, Essentials of Mini – One Anastomosis Gastric Bypass. Switzerland: Springer. 2018.
- Tolone S, Cristiano S, Savarino E, Lucido FS, Fico DI, Docimo L. Effects of omega-loop bypass on esophagogastric junction function. Surg Obes Relat Dis. 2016; 12: 62-69.
- Mion F, Tolone S, Garros A, Savarino E, Palascini E, Robert M, et al. High-resolutuon impedance manometry after sleeve gastrectomy: increased intragastric pressure and reflux are frequent events. Obes Surg. 2016; 26: 2449-2456.
- Lee WJ, Wang W, Lee YC, Huang MT, Ser KH, Chen J. Laparoscopic mini-gastric bypass: experience with tailored bypass limb according to body weight. Obes Surg. 2008; 18: 294-299.
- Jammu GS, Sharma R. A 7-year clinical audit of 1107 cases comparing sleeve gastrectomy, Roux-en-Y gastric bypass and minigastric bypass, to determine an effective and safe bariatric and metabolic procedure. Obes Surg. 2016; 26: 928-932.
- Rutledge R, Kular KS, Deitel M. Laparoscopic mini-gastric (oneanastomosis) bypass surgery. In: Agrawal S, ed, Obesity, Bariatric and Metabolic Surgery: a Practical Guide. Switzerland: Springer. 2016: 415-425.
- Lee WJ, Lee YC, Ser KH, Chen SC, Su YH. Revisional surgery for laparoscopic minigastric bypass. Surg Obes Relat Dis. 2011; 7: 486-491.
- Gagner M, Deitel M, Erickson AL, Crosby RD. Survey on laparoscopic sleeve gastrectomy (LSG) at the Fourth International Consensus Summit on Sleeve Gastrectomy. Obes Surg. 2013; 23: 2013-2017.
- Deitel M, Hargroder D, Peraglie C. Mini-gastric bypass for bariatric surgery increasing worldwide. Austin J Surg. 2016; 3: 1092- 1096.
- Peraglie C. Laparoscopic minigastric bypass (LMGB) in the super-super obese: outcomes in 16 patients. Obes Surg.2008; 18: 1126-1129.
- Peraglie C. Laparoscopic mini-gastric bypass in patients age 60 and older. Surg Endosc. 2016; 30: 38-43.
- Chen MC, Lee YC, Lee WJ, Liu HL, Ser KH. Diet behavior and low hemoglobin level after laparoscopic mini-gastric bypass surgery. Hepatogastroenterology. 2012; 59: 2530-2532.
- Scozzari G, Trapani R, Toppino M, Morino M. Esophagogastric cancer after bariatric surgery: systematic review of the literature. Surg Obes Relat Dis. 2013; 9: 133-142.
- Scheepers AF, Schoon EJ, Nienhuijs SW. Esophageal cancer after sleeve gastrectomy. Surg Obes Relat Dis. 2011; 7: 11-12.
- Angrisani L, Santonicola A, Iovino P. Gastric cancer: a de novo diagnosis after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2014; 10: 186–187.
- Felsenreich DM, Kefurt R, Schermann M, et al. Reflux, sleeve dilatation, and Barrett’s esophagus after laparoscopic sleeve gastrectomy: long-term follow-up. Obes Surg. 2017; 27: 3092– 3101.
- Wu CC, Lee WJ, Ser KH, Chen JC, Tsou JJ, Chen SC, et al. Gastric cancer after mini-gastric bypass surgery: a case report. Asian J Endosc Surg. 2013; 6: 303-306.
- Weiner RA, Theodoridou S, Weiner S. Failure of laparoscopic sleeve gastrectomy - further procedure? Obes Facts. 2011; 42- 46.
- Christou NV, Look D, MacLean LD. Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg. 2006; 244: 734-740.
- Lee WJ, Ser KH, Lee YC, Tsou JJ, Chen SC, Chen JC. Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012; 22: 1827-1834.
- Disse E, Pasquer A, Espalieu P, Poncet G, Gouillat C, Robert M. Greater weight loss with the omega loop bypass compared to Roux-en-Y gastric bypass: a comparative study. Obes Surg. 2014; 24: 841-846.
- Kular KS, Manchanda N, Rutledge R. Analysis of the five-year outcomes of sleeve gastrectomy and mini gastric bypass: A report from the Indian sub-continent. Obes Surg. 2014; 24: 1724- 1728.
- Bruzzi M, Rau C, Voron T, Guenzi M, Berger A, Chevallier JM. Single anastomosis or mini-gastric bypass: long-term results and quality of life after a 5-year follow-up. Surg Obes Relat Dis. 2015; 11: 321-326.
- Georgiadou D, Sergentanis TN, Nixon A, Diamantis T, Tsigris C, Psaltopoulou T. Efficacy and safety of laparoscopic mini-gastric bypass. A systematic review. Surg Obes Relat Dis. 2014; 10: 984- 991.
- Milone M, Lupoli R, Maletta P, Di Minno A, Bianco P, Ambrisoni P, et al. Lipid profile changes in patients undergoing bariatric surgery: a comparative study between sleeve gastrectomy and mini-gastric bypass. Int J Surg. 2015; 14: 28-32.
- Milone M, Di Minno MN, Leongito M, Maietta P, Bianco P, Taffuri C, et al. Bariatric surgery and diabetes remission: sleeve gastrectomy or mini-gastric bypass? World J Gastroenterol. 2013; 19: 6590-6597.
- Musella M, Apers J, Rheinwalt K, Ribeiro R, Manno E, Greco F, et al. Efficacy of bariatric surgery in type 2 diabetes mellitus remission: the role of mini gastric bypass/one anastomosis gastric bypass and sleeve gastrectomy at 1 year of follow-up. A European survey. Obes Surg. 2016; 26: 933–940.
- Quan Y, Huang A, Ye M, Xu M, Zhuang B, Zhang P, et al. Efficacy of laparoscopic mini gastric bypass for obesity and type 2 diabetesmellitus: a systematic review and meta-analysis. Gastroenterol Res Pract. 2015; 152852.
- Garcia-Caballero M, Valle M, Martinez-Moreno JM, Miralles F, Toval JA, Mata JM, et al. Resolution of diabetes mellitus and metabolic syndrome in normal weight 24-29 BMI patients with one anastomosis gastric bypass. Nutr Hosp. 2012; 27: 623-631.
- Carbajo MA, Jimenez JM, Castro MJ, Ortiz-Solorzano J, Arango A. Outcomes and weight loss, fasting blood glucose and glycosylated hemoglobin in a sample of 415 obese patients, included in the database of the European Accreditation Council for Excellence Centers for Bariatric Surgery with Laparoscopic One Anastomosis Gastric Bypass. Nutr Hosp. 2014; 30: 1032-1038.
- Carbajo MA, Vazquez-Pelcastre R, Aparicio-Ponce R, Luque de Lyon E, Jimenez JM, Ortiz-Solarzano J, et al. 12-year old adolescent with super morbid obesity, treated with laparoscopic one anastomosis gastric bypass (LOAGB/BAGUA): A case report after 5-year follow-up. Nutr Hosp. 2015; 31: 2327-2332.
- Kular SK, Manchanda N, Cheema GK. Seven years of mini-gastric bypass in type II diabetes patients with a body mass index <35 kg/m2. Obes Surg. 2016; 26: 1457-1462.
MedDocs Publishers
We always work towards offering the best to you. For any queries, please feel free to get in touch with us. Also you may post your valuable feedback after reading our journals, ebooks and after visiting our conferences.